35 year female born in a lower socio economic class lost her father at childhood. She started going to work since very young age. She is younger child to her parents who had two sons before her. Her younger brother suffered from CVA at young age. She loved a guy in her neighbourhood and got married to him. Her marriage life is pleasantful and had no problems.
7 years ago patient had right toe pain and took medications (unknown). Twenty days later she had CVA Rt hemiparesis . Rt upper limb recovered in three days. Lower limb recovered after three months. Later patient had complains of multiple joint pains, occasionally she took pain killers and other medications advised by RMP for her pain. 5 years later patient had complains of cough, cold and sob after getting wet in rain. She was admitted in hospital for one week for pleural effusion. for 2 years she was free from suffering and lead a normal healthy life.
In 2024 may patient had facial puffiness went to rmp and was diagnosed with Hypertension , started on medications since then
Since June patient had complains of cough, SOB, Pedal edema and came to our hospital for further management
necessary investigations were done and patient was diagnosed as autoimmune vasculitis who presented with heart failure and CKD
this is the case report of 35 year female FROM AUTOIMMUNE VASCULITIS TO MULTIORGAN FAILURE: THE DIAGNOSTIC ODYSSEY LEADING TO STROKE AND HEART FAILURE
INVESTIGATIONS
SUMMARY
C/O FACIAL PUFFINESS SINCE 2 MONTHS
B/L PEDAL EDEMA SINCE 1.5 MONTHS
SHORTNESS OF BREATH SINCE 1 MONTH
HISTORY OF PRESENTING ILLNESS:
PATIENT WAS APPARENTLY ALRIGHT 2 MONTHS AGO AFTER WHICH SHE DEVELOPED
FACIAL PUFFINESS, INSIDIOUS IN ONSET, GRADUALLY PROGRESSIVE. C/O B/L PEDAL
PITTING EDEMA, INSIDIOUS IN ONSET, GRADUALLY PROGRESSIVE FROM B/L FOOT UPTO
INGUINAL REGION AND TO ABDOMEN. C/O SHORTNESS OF BREATH SINCE 1 MONTH,
INSIDIOUS IN ONSET GRADUALLY PROGRESSIVE FROM GRADE-0 TO GRADE-3.
H/O B/L PLEURAL EFFUSION 2 YEARS AGO AND WAS ON VENTILATOR (15 DAYS) AND GOT
DISCHARGED
H/O MULTIPLE JOINY PAIN, 7 YEARS AGO STARTING IN 1ST METAPHALANGEAL TO THE
WHOLE JOINT INVOLVED, WENT TO LOCAL RMP AND TREATED WITH DEFLOCORT
PAST HISTROY:
K/C/O HYPOTHYROIDISM SINXE 2.5 YEARS AND ON THYRONORM 12.5MG
K/C/O HYPERTENSION SINCE 2 MONTHS AND ON METOPROLOL 25MG
N/K/C/O DM,CAD,TB,ASTHMA AND EPILEPSY
K/C/O HF-C MEF AND T.SACUBITRIL (24MG) + VACSARTINU (26MG)
GENERAL EXAMINATION:
PT IS C/C/C
PALLOR IS PRESENT
EDEMA IS PRESENT
NO SIGNS OF ICTERUS,CYANOSIS,CLUBBING, LYPHADENOAPTHY
TEMP: 98.6
PR:102 BPM
RR: 26CPM
BP:140/80MMHG
SPO2: 95%
GRBS:133MG%
SYSTEMIC EXAMINATION:
CVS: S1,S2 HEARD
RS: BAE+, NVBS+ Decreased breath sounds in IAA ISA
P/A: SOFT, NON TENDER
CNS: NAD
NEPHROLOGY REFERRAL DONE ON 05.07.24 I/V/O METABOLIC ACIDOSIS
ADVISED:
TAB.NODOSIS 500MG PO/TID
O2 SUPPLEMENTATION TO MAINTAIN SPO2 >95MMHG
GRBS 3RD HOURLY
STRICT I/O CHARTING
CARDIOLOGY REFERRAL DONE ON 9/7/24 I/V/O SOB ,PEDAL EDEMA AND ECG CHANGES:
ADVISED;
T.ZYTANIX 2.5 MG OD X 5 DAYS
INJ LASIX 10 ML/HR IV INFUSION
TAB ISOLAZINE TID
TAB OXRA 10 MG OD (9 AM)
INJ THYMINE 200 MG IV /OD X 5 DAYS
PLAN:MEDICAL STABILIZATION FOLLOWED BY CAG TO RULE OUT CAD
COURSE IN HOSPITAL:
PATIENT CAME WTITH ABOVE MENTIONED COMPLAINTS .2D ECHO WITH EF 42% GLOBAL
HYPOKINESIA AND DILATED CHAMBERS AND WAS STARTED ON LASIX INFUSION.PATIENT
DEVELOPED FLASH PULMONARY EDEMA AND WAS TREATED WITH INJ.NTG
.CARDIOLOGIST OPINION WAS TAKEN I/V/O HEART FAILURE WITH MIDRANGE EJECTION
FRACTION AND MEDICATION WAS STARTED AS ADVICED.HRCT WAS DONE AND SHOWED
BILATERAL PLEURAL EFFUSION,PULMONARY EDEMA AND PULMONOLOGY OPINION WAS
TAKEN AND ADVICED TO CONTINUE SAME TREATMENT.USG CHEST SHOWED THICK
SEPTUM WIITH SHALLOW FLUID POCKETS HENCE PLEURAL TAP WAS NOT DONE.ANA
PROFILE WAS SENT I/V/O POLYSEROSITIS AND REPORT WAS POSITIVE AND STARTED ON
PREDNISOLONE AND AZATHIOPRINE. AND AS THE PATIENT REQUIRES FURTHER
CARDIOLOGIST INTERVENTION AND CARDIOLOGIST ADVICE FOR CORONARY
ANGIOGRAM,HENCE THE PATIENT IS BEEN REFFERED TO HIGHER CENTRE. THE PATIENT
IS IN HEMODYNAMICALLY STABLE STATE
Investigation
HBsAg-RAPID 04-07-2024 Negative
Anti HCV Antibodies - RAPID 04-07-2024 11:45:AMNon ReactiveBLOOD UREA 04-07-2024108
mg/dl
SERUM CREATININE 04-07-2024 11:45:AM 1.5 mg/dl 1.1-0.6 mg/dl
SERUM ELECTROLYTES (Na, K, C l) 04-07-2024SODIUM 136 mmol/LPOTASSIUM 3.8
mmol/LCHLORIDE 104 mmol/L
LIVER FUNCTION TEST (LFT) 04-07-2024Total Bilurubin 0.62 mg/dlDirect Bilurubin 0.19
mg/dlSGOT(AST) 20 IU/LSGPT(ALT) 18 IU/LALKALINE PHOSPHATASE 91 IU/L
TOTAL PROTEINS 4.6 gm/dl 8.3-6.4 gm/dl
ALBUMIN 2.0 gm/dl lA/G RATIO 0.79
COMPLETE URINE EXAMINATION (CUE) 04-07-2024COLOUR Pale yellowAPPEARANCE
CloudyREACTION AcidicSP.GRAVITY 1.010ALBUMIN ++++SUGAR NilBILE SALTS NilBILE
PIGMENTS NilPUS CELLS 2-4EPITHELIAL CELLS 2-4RED BLOOD CELLS 4-6CRYSTALS
NilCASTS NilAMORPHOUS DEPOSITS Absent
ABG 04-07-2024 11:46:AMPH 7.31PCO2 19.7PO2 86.0HCO3 9.7St.HCO3 12.8BEB -15.1BEecf -
15.5TCO2 20.6O2 Sat 96.3O2 Count 12.8BLOOD UREA 05-07-2024 05:39:AM 109 mg/dl 42-12
mg/dL
SERUM CREATININE 05-07-2024 05:39:AM 1.5 mg/dl 1.1-0.6 mg/dlSERUM ELECTROLYTES (Na,
K, C l) 05-07-2024 05:39:AMSODIUM 137 mmol/L 145-136 mmol/LPOTASSIUM 4.5 mmol/L 5.1-3.5
mmol/LCHLORIDE 106 mmol/L 98-107 mmol/L
T3, T4, TSH 05-07-2024 05:39:AMT3 0.48 ng/ml 1.87-0.87 ng/mlT4 8.60 micro g/dl 12.23-6.32 micro
g/dlTSH 4.60 micro Iu/ml 5.36-0.34 micro Iu/mlBLOOD UREA 05-07-2024 11:34:PM 109 mg/dl 42-12
mg/dl
SERUM CREATININE 05-07-2024 11:34:PM 1.5 mg/dl 1.1-0.6 mg/dlSERUM ELECTROLYTES (Na,
K, C l) 05-07-2024 11:34:PMSODIUM 138 mmol/L 145-136 mmol/LPOTASSIUM 4.1 mmol/L 5.1-3.5
mmol/LCHLORIDE 104 mmol/L 98-107 mmol/L
BLOOD UREA 07-07-2024 12:57:AM 103 mg/dl 42-12 mg/dlSERUM CREATININE 07-07-2024
12:57:AM 1.7 mg/dl 1.1-0.6 mg/dl
SERUM ELECTROLYTES (Na, K, C l) 07-07-2024 12:57:AMSODIUM 138 mmol/L 145-136
mmol/LPOTASSIUM 4.3 mmol/L 5.1-3.5 mmol/LCHLORIDE 104 mmol/L 98-107 mmol/L
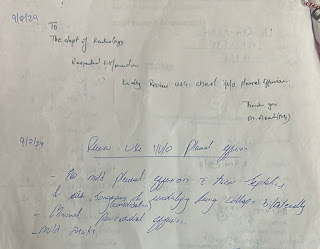
USG DONE ON 4/7/24
IMPRESION:
RIGHT PLEURAL EFFUSION WITH UNDERLYING LUNG CONSOLIDATION
LEFT PLEURAL EFFUSION WITH UNDERLYING LUNG COLLAPSE AND CONSOLIDATION
MINIMAL PERICARDIUAL EFFUSION
MILD ASCITES
USG DONE ON 9/7/24
IMPRESION: MILD PLUERAL EFFUSION WITH THICK SEPTATIONS AND AIR SONOGRAM
(CONSOLIDATION) AND UNDERLYING LUNG COLLAPSE B/L
MINIMAL PERICARDIUAL EFFUSION
MILD ASCITES
2D ECHO ON 4/7/24
CONCLUSION :MODERATE MR + ;MODERATE AR+; MODERATE TR +; WITH MILD PAH
GLOBAL HYPOKINETIC; NO AS/MS; SCLEROTIC AV
MODERATE LV SYSTOLIC DYSFUNCTION +
NO DIASTOLIC DYSFUNCTION; NO LV CLOT
HRCT OF CHEST DONE ON 10.07.24
IMPRESSION: PERIHILAR OPACITIES IN ALL LOBES OF BOTH LUNGS--- F/S/O PULMONARY
EDE,A
D/D: PULMONARY INFECTION
BILATERAL MODERATE PLEURAL EFFUSION (RIGHT >LEFT)
PROMINENT CARDIAC CHAMBERS.
ANA 17B TEST:[ ON 10/7/24]
RESULT:
ANA BLOT TEST REPORTED POSITIVE AS ANTIBODIES DETECTED AGAINST FOLLOWING
ANTIGENS FROM ANA BLOT PROFILE:
SMD1 ANTIGEN WITH AN INDEX 9.17 AND INTERPRETATION(+++)
U1 SNRNP ANTIGEN WITH AN INDEX 8.79 AND INTERPRETATION(+++)
PO(RPP)ANTIGEN WITH AN INDEX 8.56 AND INTERPRETATION(+++)
NUCLEOSOME ANTIGEN WITH AN INDEX 3.58 AND INTERPRETATION(++)
DSDNA ANTIGEN WITH AN INDEX 1.93 AND INTERPRETATION(+)
HISTONE ANTIGEN WITH AN INDEX 1.79 AND INTERPRETATION(+)
SS-A/RO60 ANTIGEN WITH AN INDEX 1.30 AND INTERPRETATION(+)
DIAGNOSIS
AUTOIMMUNE VASCULITIS
HEART FAILURE WITH MID RANGE EJECTION FRACTION
FLASH PULMONARY EDEMA (RESOLVED)
ACUTE KIDNEY INJURY
MICROCYTIC HYPOCHROMIC ANEMIA
K/C/O HYPERTENSION SINCE 2 MONTHS
K/C/O HYPOTHYROIDISM SINCE 2.5 YEARS
Treatment Given(Enter only Generic Name)
INTERMITTENT CPAP
IV FLUIDS NS @ 50ML/HR
INJ.PAN 40MG IV/OD
INJ.LASIX 100MG +40ML NS @ 5ML/HR
TAB AZATHIOPRIN 50 MG PO/OD
TAB PREDNISOLONE 40 MG PO/OD
INJ.AUGEMNTIN 600MG IV/BD
INJ.THIAMINE 200MG IN 100ML NS IV/BD
TAB..THYRONORM 12.5MICRO G PO/OD
T.CARDIVAS 3.125MG PO/OD
T.ECOSPIRIN AV 75/10 PO/HS
T.METOLAZONE 2.5MG PO/OD AT 1 PM
T.PAPAGLIFOZIN 10MG PO/OD AT 9AM
TAB IVABRADINE 5 MG PO /SOS
SYP.GRILLINCTUS DS 15ML PO/TID
NEBULISATION WITH IPRAVENT, MUCOTRIST: 8TH HOURLY AND BUDECORT:12TH HOURLY
T.OROFER XT PO/OD 0-1-0
T.NODOSIS 500MG PO/TID
T.ULTRACET PO/QID 1/2-1/2-1/2-1/2
STRICT I/O CHARTING
MONTIOR VITALS AND INFORM SOS
Advice at Discharge
1.TAB.AZATHIOPRINE 50 MG PO/OD
2.TAB.PREDNISONE 40 MG PO/OD
3.TAB.THYRONORM 12.5 MICROGRAM PO/OD
4.TAB.OROFER-XT PO/OD
5.TAB.CARDIVAS 3.125MG PO/OD
6.TAB.ECOSPIRIN AV 75/10 PO/HS
7.TAB.NODOSIS 500 MG PO/TID
8.TAB.DAPAGLIFOZOLIN 10 MG PO/OD AT 9 AM
9.TAB.ULTRACET 1/2 TAB PO/QID
10.TAB.PAN 40 MG PO/BBF
11.TAB.METAZOLINE 2.5 MG PO/OD AT 1 PM
12.TAB.TORSEMIDE 10 MG PO/OD 8AM-X-4PM
13.ADVICE FOR COMPLEMENT SYSTEM TESTING(C3,C4)
Follow up-
Patient wasn’t able to afford her medications and admitted in Govt hospital Hyderabad with complains of generalised body swelling, she was told her Hb was 2gm/dl and was given supportive care. After 10 days of admission she had her last breath and was declared dead













Comments
Post a Comment