74 male from jalalpuram came with complaints of sob and chest pain since 3 days
Patient was born and brought up in jalalpuram,lived along with parents and 3 siblings,studies till 9th standard,no health issues in childhood, discontinued education and entered carpenter work at 16 yrs of age.
He got married at age of 21 years and had 3 sons and 1 daughter and lead a relatively healthy life,
Patient remained asymptomatic till 14 years ago then he developed tingling sensation and weakness of limbs intermittently for which he went to local hospital and was diagnosed of having high blood pressures around 200/100 and was started on anti hypertensives,he was continuing medication and his bp was under control and remained asymptomatics until 7 yrs ago,
At that time he had h/o burning micturition along with pain and dribbling of urine ,he went to local hospital for that and was diagnosed of having prostatic carcinoma and resection of tumor was done at that time and also used medication for 2 years,in between he went to warangal as he was unsatisfied with the treatment of doctors there and went to warangal for further treatment as the symptoms like polyuria,burning micturition persisted even after surgery,there he was found to have recurrence of prostatic carcinoma and placed him on medical management,
Since then he was on medication for carcinoma and hypertension,
2 months ago patient developed weakness of limbs for which he went to hospital and found to have high blood sugars and was started on oral hypoglycemics,during that time he had itching over limbs and accidentally ruptured a nodule on his leg and undervent surgical procedure to close that wound
And discharged after 7 days.Since then he was worried about his health and as his financial conditions becoming worse he felt some what tensed and depressed and stopped taking medications for prostatic cancer,
Since 1 month patient noticed that he is having sob and intermittent chest pain while doing sternous work and while lifiting weights,
Sob and chest pain aggrevated since past 3-4 days for which he was brought to casuality by his attenders
No addictions
No significant family history
PHENOTYPE
Mid arm circumference- 30cms
Waist circumference- 82cms
Abdominal circumference- 87cms
Hip circumference-92cms
CHEST X-RAY PA VIEW
ECG
USH





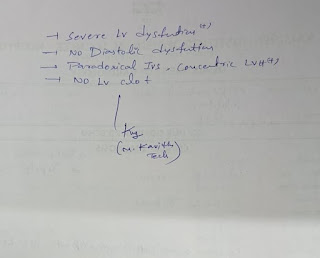
Comments
Post a Comment