Case history
40 year male autodriver by occupation resident of Narketpally came to General medicine opd with complains of Pain abdomen since 3 days, Cough since three days and Difficulty breathing since 3 days
Patient is apparently alright until 3 days ago then had complains of Epigastric pain and abdominal bloating sensation , insidious onset, intermittent , No aggravating and relieving factors. Patient consumed soda water, eno, jeera soda to alleviate symptoms
Complains of Non productive cough insidious onset associated with shortness of breath progressive from grade 1 to grade 4 aggreviated on supine position and lying on right side.
History of low grade fever not associated with chills and rigor, no diurnal variations relieved with Tab PCM650 mg
No complains of loss of appetite, weight loss, insomnia
No complains of Orthopnea, PND, Palpitations, profuse sweating
No complaints of burning micturition, increased or decreased urine output
No complains of nausea, vomiting, loose stools
PAST HISTORY
6 months ago patient had fever, body pains, tingling sensation in both hands and legs. Went to local hospital RBS was 270mg/dl and was diagnosed with Diabetes
Not a known case of HTN/THYROID/CAD/CVA/TB/EPILEPSY
30 year male born in Nalgonda to a non consanguineous marriage, father and mother were daily wage laborers. Milestones achieved normal. His younger sister was succumbed to death at 6 months old due to appendicitis. As patient parents used to stay away from home for days to months he used to migrate from his grandmothers home to aunt and their home causing disturbances to his studies. He went to private school, studied hard and passed 10th standard. At age 18 his father was diagnosed with Diabetes which made him to discontinue his studies and started working. As he learned car driving and his close circle doesn’t own an auto, it drived passion to own an auto and made it aa his occupation to drive an auto. Initially he rented the auto and deliver water cans. But as people installed home filters delivering water did not give him much profit and shifted his work to delivering vegetables to market. As days passed by he owned an auto with his hard earned money and learnt that vegetables rotten easily and he had to take frequent trips to market to deliver them unlike fruits which can still look fresh for a day or two. So he ultimately settled with fruits. In 2011 he married to his uncle’s daughter and had one elder son within an year of marriage and one daughter after three years of his marriage. In 2015 patients father was diagnosed with CVA and was treated in our hospital. Patient had taken care of his father daily needs .Patient’s father succumbed to death four years later. Since then he shouldered up all the responsibilities and took care of family of 6 members including mother wife , two children and his divorcee sister.
Daily routine
Wakes up at 5:30am walks in home and cleans his auto freshen up, drinks a glass of tea with little sugar and go to work by 8:30am. Around 10 he drinks Raagi jaava and continue his work. At 1pm he has lunch usually rice and curry. Drives auto and come back home by 7. 7-9pm he sits in his fruit store, close the store by 9pm and go home. Have his dinner usual jonna roti and a cup of tea before going to bed at 10:30pm
ON EXAMINATION
Patient is conscious coherent and cooperative
Temp- 97.6F
PR-94bpm
RR-30CPM
BP-130/90mmhg
Spo2- 99% at RA
GRBS: 128 mg/dl
GENERAL EXAMINATION
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema
RESPIRATORY EXAMINATION
UPPER RESPIRATORY TRACT
No Halitosis
Oral hygiene maintained
No oral thrush
No post nasal drip
No pharyngeal deposits
Normal tonsils
No Dental caries
Septum - Turbinate hyper trophy
No nasal polyps
No sinus tenderness
LOWER RESPIRATORY TRACT
INSPECTION
Chest is asymmetrical
Trachea appears to be central
Trails sign negative
Apical impulse not visible
Respiratory movements appreciated right side
Tactile vocal fremitus- Decreased on left side
No dropping of shoulder
Supraclavicular hollow - right side
Infraclavicular hollow absent
No intercostal fullness, indrawing, retraction, widening
No crowding of ribs
No scorbutic/rachetic rosary
No Harrisons sulcus, no pectus cavinatum/excavatum
No kyphoscoliosis/ winging of scapula
No scars, sinuses, dilated veins
No use of accessory muscles for respiration
PALPATION
All inspectory findings are confirmed
Trachea midline
No tracheal tug
Circumference
left hemithorax-51cms
right hemithorax-50cms
AP-26cms
Transverse-31.5cms
Apical impulse not felt
Chest movements decreased on left upper and lower zone
PERCUSSION
All areas resonant on percussion
No percussion tenderness
AUSCULTATION
Decreased breath sounds on left side
Vocal resonance decreased on left side
Bronchophony decreased on left side
Egophony positive on left side
Pectoriloqy decreased on left side
Succession splash negative on both sides
CVS: S1S2 Heard, No murmur
P/A: Soft, Non tender
CNS: NFND
PHENOTYPE
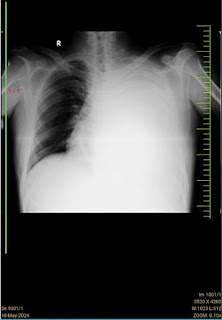
INVESTIGATIONS
PLEURAL FLUID
Cell count
Volume-2ml
Colour- colourless
Appearance- clear
Total count 2350 cells/cumm
DIFFERENTIAL COUNT
Neutrophils 5%
Lymphocytes 95%
RBC Nil
Others Nil
Sugar 144mg/dl
Protein 5 g/dl
Pleural fluid ADA 24 U/L
Pleural fluid LDH 238 IU/L
Serum LDH 210 IU/L
14/5
Pleural fluid
Sugar 166 mg/dl
Protein 4.8 g/dl
Pleural fluid LDH 8.2 IU/L
ESR 35mm/1st hour
CRP positive 2.4mg/dl
FBS 171mg/dl
PLBS. 134mg/dl
HBA1C 7%
Hemogram
Hemoglobin 12.7gm/dl
Total count 8,400 cells/cumm
N/L/E/M/B 60/30/2/8/0
PCV 36.0
RBC 4.4
Platelet 4.6 lakhs/cumm
Smear : normocytic normochromic
CUE
Albumin Nil
Sugar Nil
Pus cells 2-3
Epithelial cells 2-3
RBC Nil
Phosphorous 3.2 mg/dl
Blood urea 18mg/dl
Serum creatinine 0.8 mg/dl
Sodium 137 mmol/l
Potassium 4.1 mmol/l
Chloride 98 mmol/l
Calcium ionized 1.02mmol/l
Calcium 10.0 mg/dl
Day 1
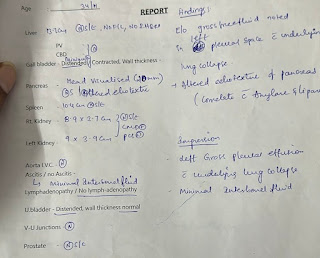
Chest X-ray
Day 2
https://youtu.be/iKZc5s_biHM?feature=shared
Day 4
X-ray DS SPINE
Day 5
https://youtube.com/shorts/mjUWX37chNI?feature=shared
PULMONOLOGY OPINION
On follow up
24-05-2024
Comparison
9/5
24/5
On follow up
17/09/2024
RBS-401
HBA1C-7.8%
27/12/2024
[26/12/24, 15:19:58] ✍🏼: RBS-180
[26/12/24, 15:20:27] ✍🏼: Patient came to today’s opd
He is on att since may
@✍️ shall we ask him to stop the medicines sir?
[26/12/24, 16:04:37] Rakesh Biswas Sir: Yes isn't it supposed to be stopped by RNTEP?
DESCRIPTION
40 year Male auto driver by occupation Diabetic admitted with complains of epigastric pain, Non productive cough associated with Shortness of breath progressive from Grade 1 to Grade 4. On auscultation there are decreased breath sounds in left side.
Chest X-ray showed massive left pleural effusion. Serum LDH:210 IU/L Peural LDH: 280 IU/L (238/210=1.33). Pleural protein:5g/dl serum protein:6.7 g/dl. (5/6.7=0.74).
Cytosmear studied shows Numerous lymphocytes, macrophages, few epitheliod like looking cells in a hemorrhagic necrotic background
We tried to measure the mediastinal shift using a 2D echo probe displacement as shown in the video attached below
https://m.youtube.com/watch?v=CYlyO0LFIck&feature=youtu.be
Typically, these shifts are observed on x-ray but also on computed tomography (CT) or magnetic resonance imaging (MRI). On chest x-ray, tracheal deviation, or movement of the trachea away from its midline position can be used as a sign of a shift. Other structures, like the heart, can also be used as reference points. [1]
REFERENCE



















Comments
Post a Comment