Chief Complaints:
Patient came to casualty with H/O 2-3 episodes of involuntary movements of right upper and lower limb and face since evening(28/10/23)
History Of Presenting Illness:
Patinet was apparently asymptomatic till today afternoon after she which she started having involuntary movements of right right upper and lower limbs associated with up rolling of eye balls and frothing not associated with involuntary micturation and defecation associated with postictal confusion for 15-20min.
H/o seizure activity on and off from past 3years and is on medication.
No h/0 fever and head trauma.
K/c/o Hypertension,CVA
Past History:
N/k/c/o DiabetesTuberculosis,bronchial asthma,epilepsy,CAD.
Personal History:
Diet : Mixed
Appetite : Normal
Sleep : Normal
Bowel and bladder moments :Regular
Addictions:None
Family History:
Not significant
General physical examination:
Patient is unconscious
Moderately built and nourished.
Temperature - 98F
PR :-78 beats per minute
BP :- 150/100mm Hg
RR:-26 cycles per minute
GRBS:-135
SpO2-90%
No precordial bulge.
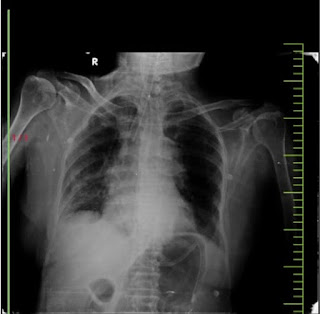
-Inspection:
Trachea -appears to be central
Chest appears bilaterally symmetrical ,movements are symmetrical on both sides.
elliptical in shape.
No chest wall defects.
No scars and sinuses.
-Palpation:
All the inspectory findings are confirmed.
Trachea central in position
-Percussion Right Left
Supraclavicular R R
Infraclavicular R R
Mammary R R
Inframammary R R
Axillary R R
Infraaxillary R R
Suprascapular R R
Infrascapular R R
R-Resonant
-Auscultation Right Left
Supraclavicular NVBS NVBS
Infraclavicular NVBS NVBS
Mammary Crepitations. NVBS
Inframammary NVBS NVBS
Axillary NVBS NVBS
Infraaxillary Crepitations. NVBS
Suprascapular NVBS NVBS
Infrascapular NVBS NVBS








Comments
Post a Comment