Thankyou anahita
A 65 year old female, resident of west bengal and belonging to middle class according to modified kuppuswamy scale presented to the general medicine OPD with chief complaints of:
-continuous dribbling of urine since the past 4 years
- constipation since past 3 years.
- shortness of breath since 3 years.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 26 years ago , when she developed:
* continuous dull aching pain in both the knee joints, which was exaggerated in the mornings and was bearable throughout the day, it was aggravated on walking and relieved on rest, associated with redness around the knees
- N/H/O trauma
- N/H/O fever with evening rise of temperature, cosmetic deformity(varicosity, skin discoloration)
- later as the disease progressed she underwent bilateral knee replacement surgery in the year 2015.
* continuous dribbling of urine since 4 years, which was insidious in onset with a few drops during the day and gradually progressed to continue throughout the day and wetting of bed during the night, urine is yellow in color with ammonical odour. Aggravated on consumption of coffee & drinking more than 1.5 lit of water.
* patient reports recurrent UTIs where in she complains of
-burning micturition
-pain before and while micturition
-no history of hematuria, frothy urine
* patient also reports constipation since 3 years,
- she passes 1 bowel movement per 2-3 days , associated with pain
- patient passes flatus
- not associated with blood, abdominal distention, weight loss
* fever since 1 day, sudden onset, high grade, continuous, no aggravating and relieving factors, associated with bodyache, headache.
HISTORY OF PAST ILLNESS:
- H/O rheumatoid arthritis since past 26yrs, is on regular medication.
- H/O HTN since past 20yrs on regular medication.
- H/O SOB since past 3years due to seasonal changes (usually in cold weather) and in stressful situations, she uses specified medication (inh. budetrol 400, oxymethazoline hydrochloride nasal drops)
-K/C/O DM since 10 days
- N/K/C/O TB, CVD, Asthma, Epilepsy, Thyroid disorders, blood transfusions.
SURGICAL HISTORY:
- history of bilateral knee replacement 8 years ago.
- history of LSCS 27yrs ago
PERSONAL HISTORY:
- Married
- Mixed diet
- Decreased appetite due to fullness of abdomen
- Adequate sleep
- Decreased bowel movement lead to constipation since past 3 yrs
- micturition: urinary incontinence since past 4yrs
- No known allergies
- no known addictions
DRUG HISTORY:
-Tab.METFORMIN 500mg
- Tab. METHOTREXATE 10mg.
- Tab. FOLIC ACID 5mg.
- Tab. CLINIDIPINE, TELMISARTAN & CHLORTHIDONE.
- Tab. BISOPROLOL FUMARATE.
- Tab. NORTRIPTYLINE, MECOBALAMIN & PREGABALIN.
- Tab. MIRABEGRON Extended release.
- Tab. RAVEPRAZOLE SODIUM 20mg & DOMPERIDONE 30mg.
- Syp. LIQUID PARAFFIN, MILK OF MAGNESIUM & SODIUM PICOSULFATE.
- Inh. BUDESONIDE.
FAMILY HISTORY:
- the patient’s mother and younger sibling are known cases of osteoarthritis
GENERAL EXAMINATION:
I have examined the patient after taking prior consent and informing the patient in the presence of a female attendant. The examination was done in both supine and sitting position in a well lit room.
Height 4feet 8inches
Weight 84kgs
Abdominal girth - 143cms
- patient was conscious, coherent and cooperative
- well oriented to time and space
- well built and adequately nourished
- no pallor
- no icterus
- no cyanosis
- no clubbing of fingers
- no lymphadenopathy
- no pedal edema
- no malnutrition
SYSTEMIC EXAMINATION:
Cardiovascular System
- no thrills
- cardiac sounds S1 and S2 heard
- no cardiac murmurs
Respiratory System
- no dyspnea
- no wheeze
- trachea position: central
- breath sounds: vesicular
- no adventitious sounds heard
Abdomen
- no tenderness
- bowel sounds heard
- no bruits, rubs
- no shifting of dullness
- no fluid thrill
- no palpable mass
- hernia orifices: normal
- liver: not palpable
- spleen : not palpable
Central Nervous System
- conscious
- normal speech
- cranial nerves normal
- motor and sensory systems normal
INVESTIGATIONS:
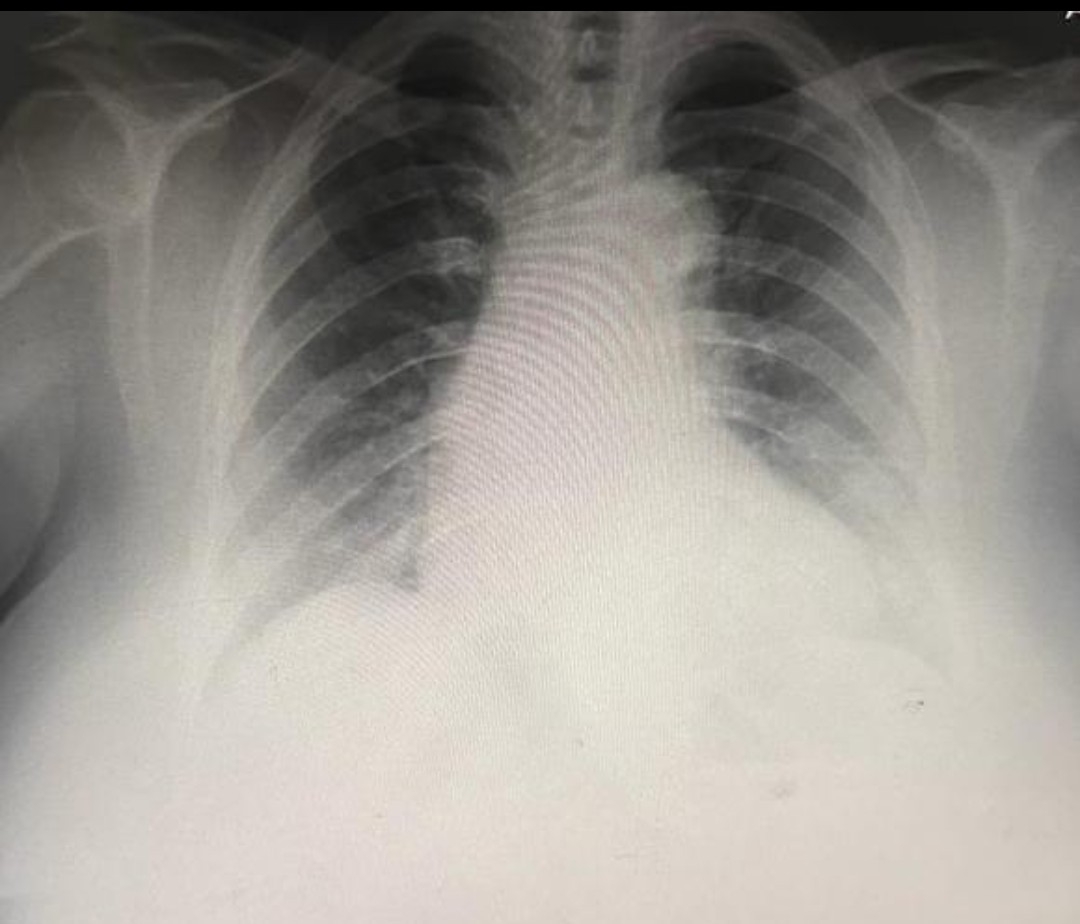
CHEST X-RAY
BILATERAL HAND X-RAY
Urology referal done on 28/09/23 I/v/o urinary incontinence while sitting /sneezing/coughing and advised Tab.SOLITEN 5MG X 2WEEKS
And USG (PVR) for bladder size
Impression: pre void -190ml
Post void-110ml
Suggestive of PVR
Urine culture sensitivity done on 29/09/23
Impression: 6-7/HPF pus cells seen and pseudomonas aeruginosa isolated
Uro metry done on 04/10/23 showing decrease in the aptitude of graph suggesting decreased force of the stream

GRBS MONITORING :
25/09/23 at 10pm : 184mg/dl
26/09/23: 2am-------8am--------11am-------2pm-------10pm-
183mg/dl-----108mg/dl----139----199------144
27/09/23:2am-------8am--------11am-------2pm-------10pm
213-----144-------200-------------140--------165
PROVISIONAL DIAGNOSIS:
UROSEPSIS (RESOLVED) SEROPOSITIVE OVER ACTIVE BLADDER (BLADDER DYSFUNCTION ) SINCE 4 YEARS WITH K/C/O RHEUMATOID ARTHRITIS (SEROPOSITIVE)SINCE 35YEARS SECONDARY TO SJOGREN'S
K/C/O CAD SINCE 26 YEARS
K/C/O HTN SINCE 20YEARS , WITH DENOVO DM2
K/C/O OSTEOARTHRITIS SINCE 20 YEARS (WITH TKR DONE)
Case 4
### Thematic Analysis of the Case
#### 1. **Coding:**
- **Chronic Conditions:** Rheumatoid arthritis, hypertension, urinary incontinence, constipation, shortness of breath (SOB), diabetes mellitus, seasonal exacerbation of symptoms.
- **Acute Symptoms:** Fever, burning micturition, continuous dribbling of urine, recurrent UTIs.
- **Surgeries:** Bilateral knee replacement, LSCS (lower segment cesarean section).
- **Family History:** Osteoarthritis in mother and sibling.
#### 2. **Categorization:**
- **Musculoskeletal Issues:** Chronic rheumatoid arthritis leading to knee replacement surgery.
- **Urinary Incontinence:** Continuous dribbling of urine, recurrent UTIs, and nocturnal bed-wetting.
- **Respiratory Symptoms:** SOB associated with seasonal changes, managed with inhalers.
- **Gastrointestinal Issues:** Chronic constipation, managed with medications.
#### 3. **Theme Identification:**
- **Multisystem Involvement in Aging:** The interplay of chronic conditions (RA, HTN, urinary incontinence) complicates the management of the patient’s health.
- **Impact of Long-Term Rheumatoid Arthritis:** Chronic joint pain, knee surgery, and ongoing management with methotrexate.
- **Patient Compliance and Autonomy:** Use of multiple medications (including for hypertension, diabetes, and SOB) shows the patient’s engagement in long-term management.
#### 4. **Theme Representation (Learning Points):**
- **Managing Chronic Multisystem Diseases in Elderly Patients:** The case highlights the complexity of managing multiple chronic illnesses, from arthritis to urinary incontinence, and the importance of a multi-disciplinary approach.
- **Recurrent Urinary Tract Infections (UTIs) as a Complication:** UTI recurrence with incontinence underscores the need for preventive measures in managing the patient’s urological issues.
- **Constipation in Elderly:** Chronic constipation and decreased bowel movements could indicate the need for lifestyle modifications and careful management of medication side effects.














Comments
Post a Comment