This is an online Elog book to discuss our patient deidentified health data shared after taking his/ her guardians sign informed consent
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with n aim to solve those patient clinical problem with collect current best evidence based input
This Elog also reflects my patient centered online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan
CHIEF COMPLAINS
Complains of stomach pain since 15 days
History of illness
Hydrocele since childhood that is from his 8 years old,increase in size unilaterally. At 12 years old he had pain at scrotum took herbal medicines, pain relieved.no pain or discomfort gradually increasing in size.
In 2011 he had sudden onset of abdominal pain, no urine output from afternoon to night with bladder fullness and sensation present. Went to local hospital and foleys was inserted. Urine output came back normal. Removed foleys and discharged after three days. Was diagnosed with BPH and advised T veltam plus.
In june 2022 he had abdominal pain, non radiating. Went to local hospital and was diagnosed with inguinal hernia.
PAST HISTORY
82 year old male resident of Malda district, farmer by occupation. wakes up at 4am freshen up; prays god for 15 minutes; reads Paper and pass stools. At 7 am the has his daily Breakfast Sattu, Moori, Dal and Apple. At 10 am he has Rice; vegetables Dal and Aloo and takes rest-for 4 hours. At 4 pm he has moori/
Rice and watches TV for 2 hours from 6pm. Dinner at 9 pm usually Dal and Rice and goes to bed.
Patient was apparently asymptomatic until 22 years ago. He fractured his 2 ribs Left side falling off bicycle and managed conservatively with belt (for 1 month).
Had artificial tooth set in 1992
Later he had episodes of abdominal discomfort once monthly relieves on taking gas tablets. Frequent cold and cough, cough-dry and occasionally productive aggravated in winter and rainy seasons; lasts for one week and relieves after taking homeopathy medications.
In 2011, abdominal pain took two painkillers and still not relieved associated with no urine output sensation present and bladder fullness present. Then visited local hospital where inserted Foleys managed with Veltamplus. Since then he’s on T.Veltamplus for 1 year paused for 4 months and later continued upon pharmacist advice. In 2014, had left eye cataract surgery and in 2015 had a cataract surgery for right eye and since then he’s using spectacles.
In February 2019, he had incomplete void of urine accompanied with frequent urination, burning micturition. Then went to local hospital and upon necessary investigation Doctor advised surgery for prostatomegaly but attenders were not willing to proceed with surgery and since then decreased input.
In 2022, abdominal pain and went to Doctor, USG showed Inguinal Hernia RT + LT, whole body was investigated and incidentally diagnosed hypothyroidism with no clinical symptoms. Abdominal pain burning sensation non radiating.
Before 2022 he is very active he does all things by himself, helps in cooking and cutting vegetables. Took care of two granddaughters till their +2.
In 2021 due to lockdown stayed at home
In may 2022 he started having stomach pain went to doctor and was diagnosed with hernia. Since then he is not able to help in household chores, cooking and taking care of granddaughters
PERSONAL HISTORY
35 years ago he joined as a disciple for guru and stopped smoking,alcohol and turned vegetarian since then.
MEDICATION HISTORY
On medications
T elotroxin 50
T veltam plus
T Doxolin AX
T Telekast L
Neurobion forte
Sunbless 60K BD
Budecort inhaler
On examination
GENERAL EXAMINATION
No pallor No icterus No lymphadenopathy No clubbing
Bilateral pedal edema pitting type
ABDOMEN
ON INSPECTION: scaphoid shaped abdomen, not distended, umbilicus inverted. No scars and sinuses
Hernial orifices: right inguinal swelling is present, cough impulse present
ON PALPATION: soft, no organomegaly, non tender
ON AUSCULTATION: Bowel sounds heard
ON PERCUSSION: Tympanic note
GENITALS
RESPIRATORY
ON INSPECTION
Barrel shaped chest
Trachea appears to be central
Bilaterally symmetrical movements, movements equal on both sides
No scars or sinus
Sebaceous cyst with discharge on posterior left infrascapular area
ON PALPITATION
Trachea centrally placed
Movements of chest equally moving on both sides
Vocal fremitus equal on both sides
ON PERCUSSION
Resonance on both sides
ON AUSCULTATION
Bilateral air entry present
CNS
Patient is oriented to time place and person
Memory intact
Speech normal
Power 5/5 in all limbs
Tone Normal in all limbs
Reflex Biceps++ triceps++ supinator+ knee++ ankle++ plantar flexion in right and left sides
OUTSIDE INVESTIGATIONS
2019
JUNE 2022
DECEMBER 2022
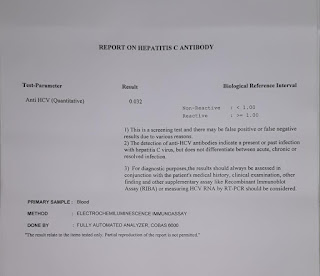
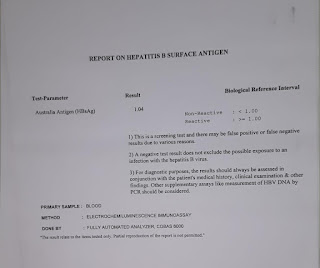
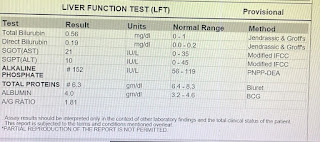
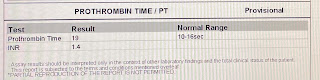
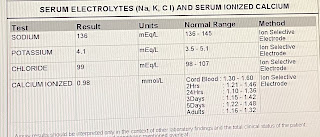
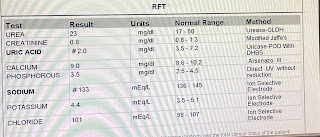
INVESTIGATIONS
9/1/23
10/1/23
16/1/23


































































Comments
Post a Comment