42/M FEVER WITH HEADACHE AND BLURRING OF VISION
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
following is the view of my case
This is a case of 42 year old male resident of kamapasagaram, Nalgonda district, working as daily wage labor presented to casualty with complains of headache and lower limb weakness since five days.
The patient initially was asymptomatic till 6 months ago. He had sudden onset of fever and SOB .
Fever without chills and rigor , no headache and nausea. Burning micturition+.
Sudden onset of SOB while working. Relieved after taking rest. He visited local hospital and was diagnosed as Hypertension with BP:200/100. On medication met-xl 25mg, chlorthalidone 12.5 mg, Telmisartan 40mg. At the same time angiogram was done which was showing mild CAD and advised medical management.
Now Complaining of Headache, blurring of vision and generalised weakness since three days.
PRESENT HISTORY:
Headache is sudden in onset localised to occipital and temporal regions, pricking type of pain. non radiating, no loss of consciousness, no nausea and vomiting, no history of seizures, no projectile vomiting. Associated with history of sudden onset of fever five days ago without chills and rigor. Fever lasted for one hour and subsided with medication. Burning micturition +. No episodes of vomitings and loose stools.
Patient was taken to private hospital miryalaguda for the same and was having high BP. Complains of blurred vision episodic lasting for few minutes or seconds.
Patient was diagnosed outside to have renal failure with a creat 5.1, urea 113, BP 200/110mmhg provisionally diagnosed with undifferentiated sepsis with AKI on ?CKD with nephropathy. CT brain showing right old lacunar infarct and was referred to our hospital for hemodialysis.
PAST HISTORY
known case of Hypertension since one year. On met-xl 25,telma 40mg, chlorthalidone 12.5mg
History of mild CAD five months ago.
PERSONAL HISTORY
Married at age of 16, has three children- one boy and two girls.
Occupation- labor
Normal appetite
Non vegetarian
Regular bowels
No known allergies
Chronic Alcoholic since 15 years. 90ml/day
FAMILY HISTORY
No significant family history.
Siblings- 5
PHYSICAL EXAMINATION
GENERAL EXAMINATION
bilateral pitting pedal edema
No pallor icterus cyanosis clubbing lymphadenopathy
Moderately nourished
VITALS
Blood pressure: 160/100mmhg
Temperature : 98 F
Pulse rate : 76bpm
Spo2: 98% at room air
GRBS :104mg/dl
SYSTEMATIC EXAMINATION
CARDIOVASCULAR SYSTEM
no thrills, no murmurs
Cardiac sound : S1 S2+
RESPIRATORY SYSTEM
No dyspnea, wheeze
Centrally placed trachea
on auscultation
ABDOMEN
No tenderness, paplpable mass, free fluid, bruits.
Normal hernial orifices
Soft, non tender, no guarding/rigidity
bowel sounds heard
CENTRAL NERVOUS SYSTEM
Conscious
Slurred speech
neck rigidity +
Signs of meningeal irritation
A) brudzinski sign - negative
B) kernigs sign- negative
Cranial nerves, motor nerves, sensory system intact
Glasgow scale- e4v5m6
Higher mental functions: Intact, no delusions or hallucinations
RT. LT
TONE: UL 4+/5 4+/5
POWER: UL. 5/5. 5/5
REFLEXES
BICEPS ++ ++
TRICEPS ++ ++
SUPINATOR ++ ++
KNEE ++ ++
ANKLE ++ ++
PLANTAR flexion flexion
Fundus examination was done and no abnormality is detected
OUTSIDE INVESTIGATIONSBrain CT was done which showed lacunar infarct (?chronic), left basofrontal lobe gliosis-sequalae, small vessel ischemic changes.
Films not available
Hb-11.2gm%
RBC-4.6milli/cumm,
TLC-12,600milli/cumm
platelet count-2.35lakhs/cumm
MCV-78.8C/M
PCV- 36.3vol%
MCH-24.4pg
MCHC-30.9mg/l
Blood urea - 103mg/dl,
s.creat- 4.9mg/dl
Na+-128mEq/L,
SGOT- 51U/L, SGPT-48U/L.
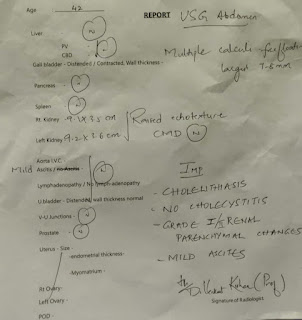
USG OF ABDOMEN: mild hepatomegaly (151mm), minimal free fuid is seen in abdomen.
INVESTIGATIONS
Day of admission
mild AR+, trivial TR+/MR+
moderate LV dysfuction+
P/A- soft, non tender
P/A- soft, non tender
DIAGNOSIS
Meningitis ?bacterial ?viral ?TB with AKI on CKD with HFmEF (EF-47%) with hyponatremia
known case of hypertension since one year
TREATMENT
1. IVF 30ml/hr
2..INJ CEFTRIAXONE 2g/IV/BD
3.TAB NICARDIA 20MG TID
4 TAB METXL 50 /OD
5 TAB TELMISARTAN-40/OD
6 TAB LASIX 40/OD
stools passed (+)
fever spikes (-)
P/A- soft, non tender
CNS- HMF intact normal gait sluured speech, no deviation of mouth NFND
7) Monitor vitals 2nd hourly, GRBS 4th hourly
P/A- soft, non tender
CNS- HMF intact normal gait normal speech, no deviation of mouth NFND
known case of hypertension since one year
P/A- soft, non tender
CNS- HMF intact normal gait normal speech, no deviation of mouth NFND
known case of hypertension since one year









































Comments
Post a Comment